Untangling Addiction: Understanding Substance Use and Pathways to Recovery
Addiction affects many Australians across all ages and backgrounds. It might begin as a way to relax after a stressful day, ease anxiety, or escape emotional pain. Over time, though, something that once offered comfort can become a pattern that feels impossible to control.
It’s important to know that if you feel like this, you’re not alone. According to the 2022–23 National Drug Strategy Household Survey, almost half of Australians aged 14 and over (47%) have used an illicit drug at some point in their lives, and nearly one in five (18%) used one in the past year. In 2023–24, over 130,000 Australians accessed publicly funded alcohol and other drug treatment services (AIHW, 2024).
Despite how common substance use is, many people still experience shame, stigma, or self-blame. Understanding addiction as a complex psychological and emotional process helps create space for compassion, recovery, and hope.
Understanding Addiction: More Than Just a Habit
Addiction changes the way the brain’s reward system functions. Substances such as alcohol, nicotine, and drugs flood the brain with dopamine, the “feel-good” chemical linked to pleasure and motivation. Over time, the brain adapts, requiring more of the substance to feel the same effect making stopping or reducing use increasingly difficult.
But beyond biology, addiction is deeply tied to our emotions and early life experiences. Many people use substances to soothe distress, loneliness, or a sense of emptiness.
From a schema therapy perspective, addictive behaviours can develop as coping strategies to deal with early patterns of belief about ourselves and the world around us (known as schemas) such as:
Feeling unlovable or defective
Fearing abandonment or rejection
Believing our needs don’t matter
Feeling unsafe or unsupported
When these core beliefs are triggered, substances can offer temporary relief from painful emotions. Unfortunately, this short-term coping can reinforce the very schemas that keep people feeling trapped.
Recognising these emotional roots of addiction shifts the focus from judgment to understanding. It allows us to see substance use as a coping mechanism that once made sense even if it now causes harm.
The Stages of Change: A Roadmap for Recovery
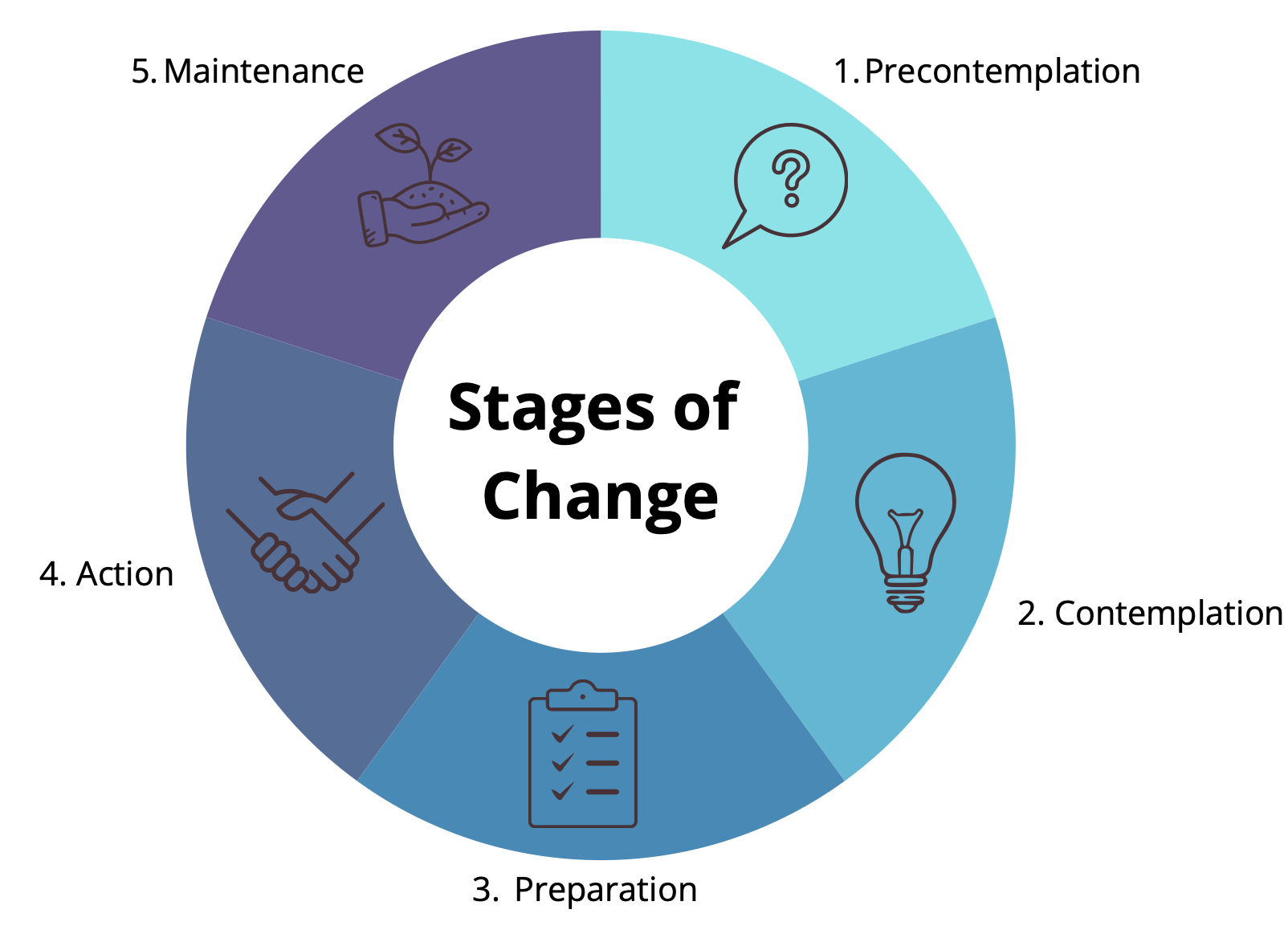
Recovery is a process, and is very rarely linear. The Stages of Change model (Prochaska & DiClemente, 1983) helps explain how people move through different phases of motivation and readiness when addressing addictive behaviours.
Stage 1. Precontemplation: The person may not yet see their substance use as a problem or may feel resigned to it. Encouragement, empathy, and gentle reflection are vital here.
Stage 2. Contemplation: Awareness begins to grow. The individual starts to recognise that substance use is causing problems and begins weighing the pros and cons of change.
Stage 3. Preparation: The person is planning to take action soon, perhaps by speaking to a GP, reaching out to a psychologist, or exploring treatment options.
Stage 4. Action: Concrete steps are taken such as entering therapy, attending support groups, or reducing substance use. Building a strong support system is key at this stage.
Stage 5. Maintenance: Sustaining recovery involves developing new routines, coping strategies, and emotional awareness. Setbacks can happen, but they are seen as opportunities for learning and recommitment.
As mentioned before, recovery isn’t linear. Moving back and forth between stages is normal. Every step, even ambivalence, represents progress toward greater awareness and self-understanding.
Pathways to Recovery
There’s no single path to recovery. What works best depends on the individual’s needs, history, and readiness for change. Effective recovery often involves a combination of medical, psychological, and community supports.
Therapeutic Support
Working with a psychologist can help uncover the emotional patterns that maintain addiction. Schema therapy, Acceptance and Commitment Therapy (ACT), and Cognitive Behavioural Therapy (CBT) are all evidence-based approaches. These therapies help individuals understand their underlying beliefs, regulate emotions, and find healthier ways to meet unmet needs.
Medical and Psychiatric Care
GPs and psychiatrists can provide crucial support for withdrawal management, prescribe medication-assisted treatments (such as naltrexone or buprenorphine), and address co-occurring conditions like anxiety or depression. Integrated care between psychologists and psychiatrists can significantly improve people’s recovery journey.
Community and Peer Support
Peer support groups offer non-judgmental environments where people can share experiences, build connection, and maintain accountability. Many local health networks across Australia provide additional harm-reduction and recovery services.
Self-Compassion and Connection
Shame often fuels the cycle of addiction. Developing compassion for oneself and understanding that substance use may have been a way to survive emotional pain can be a transformative process. Schema therapy encourages building a healthier, kinder relationship with oneself, learning to meet emotional needs through connection, creativity, and care rather than coping with substance use.
Breaking the Stigma
Addiction is often a stigmatised mental health issue. This stigma often prevents people from seeking help or speaking openly about their struggles. When we understand addiction through a trauma- and schema-informed lens, it becomes clear that it’s not a sign of weakness, but a human response to pain and disconnection. By replacing judgment with empathy and understanding, we help remove the barriers that keep people isolated in their addiction.
Final Thoughts
Addiction is not a life sentence, it’s a sign that something deeper needs attention and care. Whether you’re contemplating change or already on your recovery journey, each step forward matters. Healing takes time, patience, and support, but it’s entirely possible.
If you or someone you know is struggling with substance use, help is available:
Schema Therapy Institute Australia: (03) 9331 2878
Alcohol and Drug Foundation (ADF) Helpline: 1300 85 85 84
Lifeline: 13 11 14 (24/7 crisis support)
References
Alcohol and Drug Foundation (2024). Understanding Substance Use and Addiction. Retrieved from https://www.adf.org.au
Australian Institute of Health and Welfare (2024). Alcohol, Tobacco & Other Drugs in Australia 2024. Retrieved from https://www.aihw.gov.au
Australian Institute of Health and Welfare (2024). National Drug Strategy Household Survey 2022–23: Key Findings. Retrieved from https://www.aihw.gov.au
Marlatt, G. A., & Donovan, D. M. (2005). Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. Guilford Press.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and Processes of Self-Change of Smoking: Toward an Integrative Model of Change. Journal of Consulting and Clinical Psychology, 51(3), 390–395.
Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema Therapy: A Practitioner’s Guide. Guilford Press.